COBRA
Overview
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss, reduction in the hours worked, transition between jobs, death, divorce, and other life events.
This page is designed to help you track COBRA events and elections.
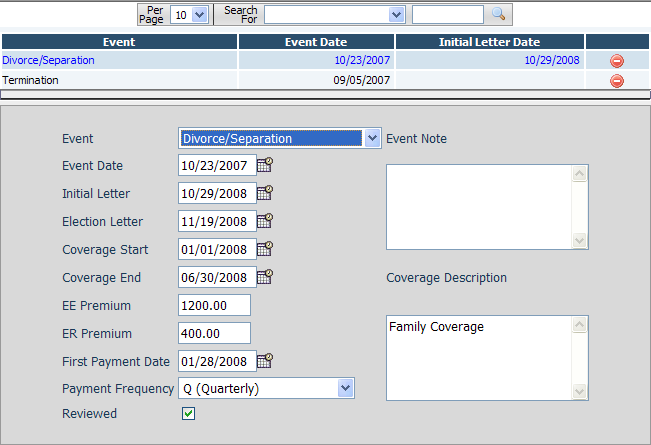
Fields
• Event – The type of qualifying COBRA event.
• Event Date – The date the qualified COBRA event occurred.
• Initial Letter – The date that the initial notification was sent to the Plan Administrator
• Election Letter – The date that the employee was sent an election notice.
• Coverage Start – The date that COBRA coverage for an employee starts.
• Coverage End – The date that COBRA coverage for an employee ends.
• EE Premium – The amount that the employee must pay for the coverage.
• ER Premium – The amount that the employer is paying for the coverage.
• First Payment Date – The date of the first employee payment.
• Payment Frequency – The frequency that the employee is making payments.
• Reviewed – A checkbox that allows you to mark the COBRA event as complete and reviewed.
• Event Note – An optional free-flowing text area for describing the COBRA event.
• Coverage Description – A free-flowing description describing the coverage the employee has elected.